In 2008, the World Health Organization’s Commission on the Social Determinants of Health released its final report, which linked inequalities in life expectancy and health status across social groups to underlying inequalities in resources and power. Drawing on decades of work by social epidemiologists, the report concluded that “social injustice is killing people on a grand scale.”
The WHO report drew on decades of academic research, domestic government reports, and the work of international organizations, all of which have contributed to a growing recognition among politicians in the rich Western democracies that inequalities in health are linked to socioeconomic inequalities.
What happens when politicians, policymakers, and even researchers begin to frame the problem of social inequality in health terms? In my research, I draw on a variety of sources and methods—in-depth interviews, archival research, network analysis, qualitative content analysis—to argue that reframing social inequality in terms of health unexpectedly reshapes the policymaking environment surrounding social inequality in ways that actually make it more difficult to reduce both social inequality and health inequalities.
The emergence of scholarly and policy research linking health inequalities to social class inequalities presents politicians with an opportunity: reframing the issue of social inequality as a problem of health allows them to embrace the issue of equity while steering away from contentious issues like redistribution of income and wealth, and drawing links to more palatable topics like attempting to rein in rapidly escalating health care costs. The most obvious linking of health and social inequality in political discourse occurred in the 1997 national election campaign in Britain, in which the Labour Party successfully used the issue of health inequalities to highlight the failure of the incumbent Conservative government’s health and economic policies. As one activist put it to me in an interview, “The way we kicked the Tories was to say that they were literally killing people. Labour absolutely loved the early health inequalities [research] because it said you are child killers, your trickle-down isn’t working.”
“Politicians and policymakers took up the issue of health inequalities for a variety of reasons.”My interview research in the United Kingdom, France, Finland, and Belgium (May 2012 to March 2015) showed that politicians and policymakers took up the issue of health inequalities for a variety of reasons. In the United Kingdom, the health inequalities problem frame, with its focus on the social determinants of health, allowed center-left policymakers to reintroduce the possibility of redistributive social policy when the neoliberal consensus of the 1980s and 1990s made consideration of such policies fraught. In Finland and France, the health inequalities issue was politically useful because it resonated with a longstanding political emphasis on social equality in their countries without directly referencing income inequality or redistribution. Raising the issue of health inequalities also was viewed by policymakers in all four countries as lending legitimacy to their attempts to reform other aspects of the health system (e.g., limiting expenditures, controlling providers or insurers, reducing geographical variation in health services consumption or supply).
Since politicians adopt health inequalities as a political problem for different reasons and with varying degrees of commitment, many aspects of the policy response to health inequalities naturally also differ across countries. Nevertheless, a standard set of widely publicized policy recommendations has been embraced by international actors such as the WHO’s Regional Office for Europe and the European Union. The four key policy recommendations are (1) coordinating multisectoral action that uses policies beyond the health sector to promote better health; (2) encouraging leadership from national governments; (3) targeting health improvements across the entire socioeconomic gradient rather than targeting only the most deprived; and (4) reducing or eliminating the fundamental inequalities in power and resources that cause health inequalities. These recommendations are consistent with the health inequalities problem frame and well understood by policymakers—so much so that I was quite surprised as my research progressed to find that even in countries where health inequality is on the political agenda, policies are often not consistent with this set of recommendations.
The gap between recognition and policy action
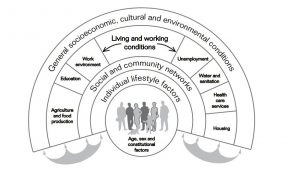
Even when key national policy documents regarding health inequalities recognize that health has social as well as medical determinants (such as the US Department of Health and Human Services’ Action Plan to Reduce Racial and Ethnic Health Disparities), government policies to reduce health inequalities often work mainly through the health sector, relying on medicalized understandings of primary care and prevention and health promotion policies targeting individuals and their behaviors rather than the structures within which these behaviors take place. In most countries, national-level coordination and oversight of policies targeting health inequalities have taken a backseat to local initiatives. Actions against poverty and marginalization have played a role in health inequalities plans from England to France to Finland, but to date only Norway among the European countries has a national health inequalities reduction program that highlights reducing income inequality as a means to reduce health inequalities. Explaining why the recommended policy strategy has not been enacted after the “health inequalities turn” can help us understand why political attention to health inequalities may undermine attempts to reduce inequality.
Some researchers have pointed to problems of public health policymaking and implementation to explain the lack of progress in combating health inequalities. Each of the four central policy elements recommended for combating health inequalities—multisectoral action, national-level leadership, action across the gradient, and action on the underlying causes—is difficult and/or counterintuitive to policymakers. So, while there is little disagreement that health inequalities and social inequalities are linked, reframing the issue of social inequality in terms of health creates a problem that might at first seem politically less difficulty, but is in many ways more complicated than “merely” reducing income inequality.
I’d like to highlight here just two of the mechanisms through which this happens: medicalization, and the creation of a “wicked problem.”
Medicalization
Medicalization of inequality occurs when health professionals come to dominate policymaking and meaning-making around the issue of inequality. But how does this happen in a paradigm that highlights the non-medical determinants of health and calls for cross-sectoral policymaking? Reducing health inequalities requires cooperation among multiple ministries and policy fields, from finance to transportation to housing to education to health, since the health system alone does not control the policy levers needed to remedy inequalities in the social determinants of health. Such cooperation is difficult, though: it requires policymakers to agree on goals and instruments, share budgets, and relinquish or take on new responsibilities.
“The medical model of health makes action on the social determinants of health less likely.”The default if such coordination does not occur—and frequently it does not, especially at the national level—is for health inequalities policy to become the “property” of the health sector. In this case, medical authorities, who tend to play a more dominant role within health systems than do public health authorities, become the key actors defining and implementing health inequalities policies. But the medical model of health, which posits the individual rather than her surroundings as the unit of analysis, makes action on the social determinants of health less likely. A belief in individualism links neoliberalism and the medical model of health, and makes the two meta-frames especially compatible. This resonance may allow neoliberal ideas to influence policy styles in institutional settings that are dominated by actors who have a medicalized understanding of health, or among public health professionals whose training and outlook is primarily biomedical rather than social.
“Wicked problems”
The second key mechanism that seems to constrain effective policymaking to combat health inequalities is the reconstruction of inequality as a “wicked problem.” As defined by policy scholars Horst Rittel and Melvin Webber in the early 1970s, wicked problems involve disputes over the definition of the public good and have no definitive solutions; evidence about how to solve the problem is often missing or uncertain; and there are numerous possible intervention points, the consequences of which are hard to foresee. Together, these characteristics create problems that are surrounded by uncertainty, and likely to seem insoluble using policy approaches within the current repertoire of policymakers.
“By highlighting the ‘wickedness’ of inequality as a policy problem, the health inequalities policy framing renders the problem of social inequality much more difficult to solve.”The health inequalities problem frame spotlights many of these troubling characteristics. The social determinants causal interpretation and the cross-sectoral treatment recommendation highlight the complexity of causation and the multiple systems that must be recruited into a solution. A focus on inequalities operating over the life-course implies that outcomes of interventions are bound to be distal. Furthermore, the moral evaluation inherent to the health inequalities problem frame—exonerating individuals and blaming market inequalities and government policies for health inequalities—brings into focus how value-laden are both the definition of and the solutions to the problem of health inequalities. By highlighting the “wickedness” of inequality as a policy problem, the health inequalities policy framing renders the problem of social inequality much more difficult to solve. By comparison, the more traditional approach to inequality as an economic problem comes with a relatively straightforward set of policy tools (taxation, redistribution, labor market regulation) that produce relatively well-understood outcomes in a relatively short period of time.
Of course, reducing income inequality is politically difficult. Recall that a desire to avoid discussing redistribution provides the motivation for at least some politicians to highlight health inequality as their signature issue. As one British policymaker explained to me, “The Labour government didn’t want to explicitly address income inequality. They would never have framed what they were doing in terms of reducing the gap between the rich and the poor. That would be political suicide.” Another said, “[Labour] are keen to talk about health inequalities providing they don’t have to talk about income and wealth inequalities.” Even in Finland, where social solidarity is a value shared across the political spectrum, “for the Right it’s easier to emphasize their pro-equality position by talking about health inequalities, because it doesn’t concern distributing income, which is a more difficult for them.” Constraints on macroeconomic policy deriving from corporate lobbying, domestic and international financial markets, or international financial institutions could also contribute to reticence about implementing bold redistributive policies designed to reduce inequalities in the upstream determinants of health.
Conclusion
In sum, health inequalities may be a politically appealing problem frame, making palatable certain proposals to reduce inequality that would be politically infeasible if posed baldly as redistribution. But reframing social inequality as a problem of health introduces a great deal of complexity, perhaps even “wickedness.” This framing implies a need for difficult coordination across policy sectors, and makes the problem at hand seem unamenable to policy intervention, all of which makes it more difficult to combat the power of neoliberal ideas and actors already present within the policymaking arena. These institutional and political obstacles help to explain why, even when policymakers adopt and promote the problem of health inequalities in part in order to address the underlying inequalities, this problem frame can fail to produce a policy response that would redress either health inequalities or the fundamental causes of these inequalities.
Where does this leave political actors who might have hoped to use the health inequalities frame strategically, as a way to reintroduce redistributive policy after three decades of neoliberal hegemony? Policymakers interested in reducing either social inequalities or health inequalities would do well to eschew the health inequalities problem frame and instead adopt a more “traditional” plan for reducing social inequality consisting of taxation, redistribution, and labor market regulation. These policies may seem too politically risky to consider, and near impossible to enact in a neoliberal era; but they have the benefit of being relatively straightforward to imagine and to implement by a single ministry.













